 |
 |
| Encephalitis > Volume 3(2); 2023 > Article |
|
Abstract
Purpose
Toxoplasma gondii is a parasite that is widely distributed around the globe and can cause brain inflammation, particularly in immunosuppressed patients such as those diagnosed with human immunodeficiency virus (HIV). This paper reviews the efficacy of azithromycin and pyrimethamine combination therapy for cerebral toxoplasmosis in patients with HIV.
Methods
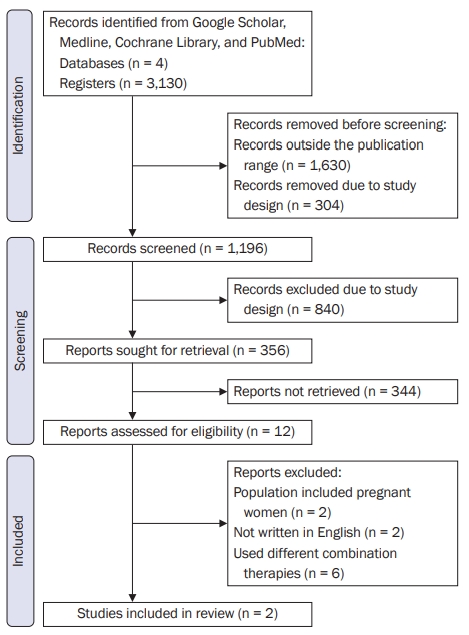
The scope of the studies included in this review was limited from 1992 to 2022, with studies primarily being randomized, controlled clinical trials available on online scientific journal databases. The authors screened eligible records for review, removing those that did not fit the inclusion and exclusion criteria. The risk of bias of the extracted data was analyzed through the Cochrane risk-of-bias tool for randomized trials.
Results
A broad search of major online databases such as PubMed, Medline, Google Scholar, and Cochrane using keywords, limit fields, and Boolean operators yielded 3,130 articles. After thoroughly screening the search results, two studies were included in this review. Results from the studies included in the review demonstrate that the combination therapy of azithromycin and pyrimethamine is favorable for cerebral toxoplasmosis. However, the net response is less effective than the standard treatment regimen (pyrimethamine and sulfadiazine).
Toxoplasma gondii is an abundant, intracellular protozoan parasite that causes zoonotic infection [1] that has affected individuals all around the world. The geographic distribution of T. gondii varies greatly. Africa, South America, and Western Europe all have higher parasite prevalence rates [1]. A third of the worldŌĆÖs population, including more than 13 million human immunodeficiency virus (HIV)-positive individuals, are infected with T. gondii, which causes brain inflammation and a number of other disorders [2].
Infection with T. gondii can be acquired through the consumption of raw meat containing parasitic tissue cysts, oocyst consumption from cat feces that have been infected, blood transfusion using contaminated leukocyte preparations, unintentional laboratory inoculation, organ transplantation, or transplacental contamination [3].
Fortunately, in those with healthy immunity, toxoplasmosis is often a self-limiting condition. However, immunocompromised persons, such as patients with AIDS and the fetuses of women who have had a primo-infection, are at increased risk of developing severe toxoplasmosis [4]. Unifocal or multifocal lesions, which are more frequent, and diffused encephalitis are symptoms of cerebral toxoplasmosis. Patients often display subacute symptoms; however, symptoms are acute in around 10% of cases. Clinical signs and symptoms vary by area and number of lesions. Headache (49%ŌĆō63%), fever (41%ŌĆō68%), focal impairment (22%ŌĆō80%), seizures (19%ŌĆō29%), and mental problems are among the more common symptoms. Disorientation (15%ŌĆō52%), ataxia (15%ŌĆō25%), lethargy (12%ŌĆō44%), changes in the cranial nerves (12%ŌĆō19%), and changes in vision (8%ŌĆō15%) are some of the other symptoms [5].
For patients with compromised cellular immunity, such as those who have HIV infection or are taking immunosuppressive or cancer treatment, toxoplasmosis is a potentially fatal condition. Reactivation of a chronic infection rather than newly acquired infection is the main cause of sickness in this population. Reactivation of previously acquired Toxoplasma infection in the form of cerebral encephalitis is more likely to occur in immunocompromised patients. Moreover, continuous medication is necessary for immunocompromised individuals to control progressive illness and to avoid recurrence [6].
The most often prescribed drugs for treatment of T. gondii infection include pyrimethamine and sulfadiazine. Pyrimethamine alone in high doses or in combination with clindamycin, clarithromycin, azithromycin, or atovaquone can be used as a replacement for patients with sulfonamide hypersensitivity [7]. Azithromycin and other macrolide antimicrobials have proven to be effective in treating toxoplasmic encephalitis in animal models, and their combination with pyrimethamine has also been shown to have synergistic effects [8]. Moreover, a study done by Huskinson-Mark et al. [9] demonstrated azithromycin to be effective in vitro against T. gondii cysts, which are thought to represent the root cause of recrudescent infection in AIDS patients.
Furthermore, some meta-analysis studies used clindamycin with pyrimethamine and sulfadiazine to treat cerebral toxoplasmosis; however, given the pharmacokinetics of azithromycin and clindamycin, it was noted that azithromycin, a basic, highly lipophilic compound, has a relatively high molecular mass and penetrates more readily into tissue [10]. Additionally, it penetrates readily into brain tissue and appears to be widely distributed to brain tissue [11]. In comparison, clindamycin, a lincosamide antibiotic, is a small lipophilic compound that possesses a small molecular mass and is highly bound to plasma proteins. Its central nervous system (CNS) absorption is regarded as being unsatisfactory, though it can reach a therapeutic cerebrospinal fluid concentration from a high dose [11]. Likewise, since azithromycin is readily available and has a low level of toxicity, we thought of its use to treat cerebral toxoplasmosis [12].
To address concerns regarding the treatment efficacy of a combination of azithromycin and pyrimethamine for the therapy of cerebral toxoplasmosis, a systematic review of the literature for their combined use in treatment of cerebral toxoplasmosis or toxoplasmosis encephalitis was conducted. Because different groups of people may need different therapeutic drugs, the treatment of T. gondii infection in patients with HIV infection was specifically analyzed here. Furthermore, adverse reactions (AEs) from using azithromycin as part of the therapy for cerebral toxoplasmosis in patients with HIV were also reviewed.
This systematic review was conducted in accordance with the PRISMA StatementŌĆÖs guidelines. Google Scholar, Medline, Cochrane Library, and PubMed, were searched by combing the terms ŌĆ£CNS ToxoplasmosisŌĆØ or ŌĆ£ToxoplasmosisŌĆØ and ŌĆ£AzithromycinŌĆØ or ŌĆ£Azithromycin with pyrimethamineŌĆØ and ŌĆ£treatmentŌĆØ or ŌĆ£therapyŌĆØ. The published languages and years were limited to 15 years, and published studies were performed with human subjects.
Studies were included if they fulfilled the criteria as follows: (1) it was a cohort study; (2) patient was diagnosed with HIV and the diagnosis of HIV infection was based on a serological examination for HIV; (3) patient was diagnosed with T. gondii infection and the diagnosis of T. gondii infection was based on a serological examination for T. gondii antibodies (immunoglobulin [Ig] G and/or IgM), parasite observation, or polymerase chain reaction (PCR) detection of DNA; (4) a positive result was represented by the presence of IgM, IgA, significant increase in specific IgG or a positive parasite observation, and a positive PCR result in detection of T. gondii DNA; (5) the diagnosis of cerebral toxoplasmosis was confirmed by computed tomography (CT) or magnetic resonance imaging (MRI) scans and neurological clinical signs or symptoms, which included headache, seizures, changes in sensorium, hemiplegia or hemiparesis and hemi sensory loss; (6) studies that evaluated the subjects by clinical and radiological responses; (7) studies that monitored and recorded the adverse effects of azithromycin and pyrimethamine; and (8) studies that were published from 1992 to 2022 and were written in English.
Studies were excluded if they were described by the following criteria: (1) studies that were case series, literature reviews, and case reports; (2) studies that used other combinations of medication other than azithromycin and pyrimethamine; (3) studies that used pediatric patients (0ŌĆō18 years of age) and pregnant patients; (4) duplicated data from other studies; and (5) studies that were published before 1992 and were not written in English (Appendix 1).
Each studyŌĆÖs initial author, publication date, sample size, diagnostic techniques, medication, and dose information were collected. The researcher identified which studies to include in the systematic review based on the given inclusion and exclusion criteria.
The results of this systematic review were assessed via the Cochrane risk-of-bias tool for randomized trials to reinforce the certainty of the evidence (Figure 1).
After a thorough selection process, only two articles matched all of the details outlined in the inclusion criteria. From 3,130 original hits across four databases, 1,630 articles were removed because they were published outside of the desired publication range. Another 1,144 were removed due to inconsistencies with the study design (e.g. case reports, case studies, and systematic reviews). Of the 12 remaining eligible studies, two articles were removed because their population included pregnant women; two studies were excluded because they were written in a language other than English; and six studies were removed because they used different combinations of therapies other than azithromycin and pyrimethamine.
Table 1 shows the summary of results from the two pooled articles, including details about the first author, publication year, sample size, drug dosage, and evaluation using the Cochrane risk-of-bias tool for randomized trials.
Table 2 shows a summary of common adverse events experienced by the subjects in both trials. Adverse events were evaluated by clinical manifestation and laboratory parameters. Most of the common adverse events noted were rashes, increase in liver enzymes, nausea and vomiting, and hearing loss.
Evidence from randomized controlled clinical trials, on treatment for cerebral toxoplasmosis using azithromycin or a combination of azithromycin and pyrimethamine is limited; hence, the grade of recommendations that can be made based on the evidence provided is low. While the quality of the trials was methodologically sound, there is the risk of bias on the effect of adherence and the small population size, as shown in Table 3. Likewise, the risk of bias on the reporting part is low since both protocols were cleared and expected outcomes of interest were reported.
In summary, the risk of bias for both studies was high, with the main risk being the limited number of evaluable patients and the effect of patientsŌĆÖ adherence to the intervention. Shown in Table 3 is a summary of risk of bias analysis.
In the study of Saba et al. [13], 14 patients diagnosed with AIDS, aged 20 to 55 years, were enrolled in the trial. Of the 14 subjects, only seven subjects were able to complete the 28-day regimen as scheduled, while the other seven subjects discontinued azithromycin therapy due to the occurrence of adverse events in five patients, uncontrolled toxoplasmic encephalitis in one patient, and a hospital transfer for another patient.
These patients were assessed clinically and neurologically from day 1 to day 7; they were then evaluated on a weekly basis thereafter. Prior to and after the initiation of azithromycin therapy, a CT scan or MRI was done. Clinical and radiological responses were graded independently. Specifically, if a complete or partial response (>50% improvement) was observed, the outcome was deemed favorable. If an incomplete response (<50% improvement) was observed, the outcome was deemed intermediate. If no improvement or worsening of clinical or radiological signs occurred, the outcome was classified as unfavorable.
Among patients who received azithromycin treatment for more than 21 days, eight were evaluable for clinical response, while two patients had seizures as the clinical manifestation of encephalitis. Of these eight evaluable patients, five patients had favorable responses, while one patient displayed an intermediate response. Nine patients were evaluable for radiologic response; six had favorable responses while three had intermediate responses.
In the same study, five patients developed a skin rash that was postulated to be due to azithromycin in four patients and pyrimethamine in one patient. Meanwhile, vomiting also occurred in three patients; however, its relationship with azithromycin could not be documented with certainty because the patient died. Overall, adverse events required discontinuation of the protocol in five of the 14 patients.
In the study of Jacobson et al. [8], the authors enrolled 42 adult HIV-infected patients with confirmed acute toxoplasmic encephalitis. The subjects were divided into three cohorts, with escalating doses of azithromycin in each. Specifically, the cohorts received 900 mg, 1,200 mg, or 1500 mg of azithromycin a day. The induction period lasted for 6 weeks, followed by maintenance therapy for 24 weeks.
Physical examination and a complete blood count were conducted at entry, then weekly for the first 6 weeks, then monthly thereafter. Patient response was then evaluated through the use of a standardized neurological examination, which consisted of objective criteria that allowed for assessment of the patientŌĆÖs neurological status at each evaluation point.
Responses to therapy were categorized into clinical and radiological. Complete clinical response at induction period was defined as a complete resolution of all abnormal CNS signs and symptoms, which were attributed to toxoplasmosis. Meanwhile, partial response was defined as a definite improvement in any symptom without complete resolution of all abnormal CNS signs and symptoms. Failure in therapy was further categorized into (a) no change, in which there was no clinical improvement or deterioration, without new neurological abnormality by 6 weeks; and (b) progression, in which there was an increasing severity of any or all neurological signs, or a new neurological abnormality within 6 weeks.
Radiological response at induction period was also divided into complete response, partial response, and failure. Complete response constituted a normal CT or MRI, while partial response referred to no new lesions or increase in size of predetermined lesions. Failure referred to no change, no new lesions, or an increase in size of previous lesions or progression, in which there was an appearance of new lesions.
Of the 40 patients who received therapy for 6 weeks, 10 were not evaluable for efficacy, five were subsequently determined to be seronegative for toxoplasma, three had other CNS pathologies (specifically: Nocardia, CNS lymphoma, meningitis), and two requested withdrawal before being evaluated for response. Of the 30 evaluable subjects, 20 (67%) responded to acute study treatment, while 10 subjects (33%) experienced disease progression during the induction period. Seven of 15 responders who received maintenance therapy after week 6 relapsed, one discontinued due to toxicity, and one withdrew from the study.
Seven patients experienced adverse effects, thereby requiring discontinuation of study medication. Two patients had elevated serum glutamic-pyruvic transaminase at week 3, another had a grade IV increase in gamma-glutamyltransferase at week 5. Two patients experienced grade II nausea and vomiting, resulting in their voluntary withdrawal from the study during week 2. Two other patients experienced hearing loss.
From the two studies included in this systematic review, there is reasonable evidence that the effect of azithromycin plus pyrimethamine therapy on cerebral toxoplasmosis is favorable in patients with HIV. However, despite favorable responses, the overall response rate in these two studies was less than the 77% to 79% favorable response rate that is achieved with conventional treatment [14]. As such, the use of azithromycin and pyrimethamine appears to be less effective than the standard treatment regimen of pyrimethamine and sulfadiazine.
In conclusion, the use of azithromycin and pyrimethamine in the treatment of cerebral toxoplasmosis appears to be less effective than the standard treatment regimens as maintenance therapy for cerebral toxoplasmosis. However, the interpretation of this review must be approached with caution and must be moderated by the fact that studies on this treatment regimen are limited. Moreover, the existing studies have limited evaluable patients and thus have high risks of bias.
Furthermore, adverse events developed in a number of patients using the study treatment of azithromycin. However, to which drug AEs must be attributed is inconclusive because the AEs may have also been caused by pyrimethamine. In addition, the rate of toxicity associated with the combination therapy of azithromycin and pyrimethamine is deemed similar to AEs associated with the standard regimens. As such, the rate of adverse events in relation to the combination therapy of azithromycin and pyrimethamine appeared to be acceptable in the studies encompassing cerebral toxoplasmosis.
Limitations of this review include the limited number of studies included as well as the small sample size of the studies. Furthermore, most studies are case reports, and used different combinations of medications, thus recommendations for future research include considering larger sample sizes with homogenous doses of antimicrobials and duration of treatments in randomized and controlled studies to draw stronger conclusions.
Table┬Ā1
Summary of findings of pooled trials
| Study | Year | Population (n) | Drug dosage (mg) | Clinical response | Radiological response | RoB 2 |
|---|---|---|---|---|---|---|
| Saba et al. [13] | 1993 | 14 | Azithromycin 500 + pyrimethamine 75 | 62.5% favorable | 66.7% favorable | Moderate |
| Jacobson et al. [8] | 2001 | 42 | (i) Azithromycin 900 + pyrimethamine | 67% favorable | Moderate | |
| (ii) Azithromycin 1,200 + pyrimethamine | ||||||
| (iii) Azithromycin 1,500 + pyrimethamine | ||||||
Table┬Ā2
Summary of common adverse events in both trials
| Study | Year | Drug dosage (mg) | Adverse events | No. of subjects (%) |
|---|---|---|---|---|
| Saba et al. [13] | 1993 | Azithromycin 500 + pyrimethamine 75 | Rash | 5 (36) |
| Abnormalities in liver tests (3ŌĆō6 fold normal levels) | 2 (14) | |||
| Vomiting | 3 (21) | |||
| Hypoacousia | 1 (7) | |||
| Jacobson et al. [8] | 2001 | (i) Azithromycin 900 + pyrimethamine | Increase in SGPT/SGOT (>5├Ś upper normal limit) | 4 (10) |
| (ii) Azithromycin 1,200 + pyrimethamine | Increase in GGT (>5├Ś upper normal limit) | 3 (7) | ||
| (iii) Azithromycin 1,500 + pyrimethamine | Anemia (<7 g/dL) | 3 (7) | ||
| Nausea and vomiting | 2 (5) | |||
| Fever | 2 (5) | |||
| Hearing loss | 2 (5) |
Table┬Ā3
Summary of risk of bias analysis using the RoB 2 method
| Study | Year |
Domain 1 |
Domain 2 |
Domain 2 |
Domain 3 |
Domain 4 |
Domain 5 |
|---|---|---|---|---|---|---|---|
| Randomization | Effect of Assignment | Effect of Adherence | Attrition | Detection | Reporting | ||
| Saba et al. [13] | 1993 | Low | Low | High | Some concerns | Low | Low |
| Jacobson et al. [8] | 2001 | Low | Low | Low | Low | Low | Low |
References
1. Vidal JE. HIV-related cerebral toxoplasmosis revisited: current concepts and controversies of an old disease. J Int Assoc Provid AIDS Care 2019;18:2325958219867315.



2. Dian S, Ganiem AR, Ekawardhani S. Cerebral toxoplasmosis in HIV-infected patients: a review. Pathog Glob Health 2023;117:14ŌĆō23.



3. Shiojiri D, Kinai E, Teruya K, Kikuchi Y, Oka S. Combination of clindamycin and azithromycin as alternative treatment for Toxoplasma gondii encephalitis. Emerg Infect Dis 2019;25:841ŌĆō843.



4. Chang HR. The potential role of azithromycin in the treatment of prophylaxis of toxoplasmosis. Int J STD AIDS 1996;7 Suppl 1:18ŌĆō22.


5. Pereira-Chioccola VL, Vidal JE, Su C. Toxoplasma gondii infection and cerebral toxoplasmosis in HIV-infected patients. Future Microbiol 2009;4:1363ŌĆō1379.


6. Rajapakse S, Chrishan Shivanthan M, Samaranayake N, Rodrigo C, Deepika Fernando S. Antibiotics for human toxoplasmosis: a systematic review of randomized trials. Pathog Glob Health 2013;107:162ŌĆō169.



7. Wei HX, Wei SS, Lindsay DS, Peng HJ. A systematic review and meta-analysis of the efficacy of anti-Toxoplasma gondii medicines in humans. PLoS One 2015;10:e0138204.



8. Jacobson JM, Hafner R, Remington J, et al. Dose-escalation, phase I/II study of azithromycin and pyrimethamine for the treatment of toxoplasmic encephalitis in AIDS. AIDS 2001;15:583ŌĆō589.


9. Huskinson-Mark J, Araujo FG, Remington JS. Evaluation of the effect of drugs on the cyst form of Toxoplasma gondii. J Infect Dis 1991;164:170ŌĆō171.


10. Fohner AE, Sparreboom A, Altman RB, Klein TE. PharmGKB summary: macrolide antibiotic pathway, pharmacokinetics/pharmacodynamics. Pharmacogenet Genomics 2017;27:164ŌĆō167.



11. Nau R, S├Črgel F, Eiffert H. Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system infections. Clin Microbiol Rev 2010;23:858ŌĆō883.




12. Rothova A, Bosch-Driessen LE, van Loon NH, Treffers WF. Azithromycin for ocular toxoplasmosis. Br J Ophthalmol 1998;82:1306ŌĆō1308.



Appendices
Appendix┬Ā1.
Summary of excluded studies
- TOOLS
-
METRICS

-
- 0 Crossref
- 0
- 1,537 View
- 30 Download
- ORCID iDs
-
Mark Erving H. Ramos

https://orcid.org/0000-0002-5069-2397 - Related articles

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



